Personalized Attention to Lifestyle Factors may Reduce A-Fib Risk for Indviduals
Atrial fibrillation, or AFib, is a common arrhythmia characterized by an irregular heartbeat, posing a significant risk for strokes. While genetics, age, and sex are non-modifiable factors, lifestyle choices, comorbid conditions, and socioeconomic status play a significant role in its prevalence and complications.
Smoking, excessive alcohol consumption, physical inactivity, and obesity are lifestyle factors that raise the risk of AFib and its severity. Accordingly, adopting a heart-healthy lifestyle, including regular exercise, maintaining a balanced diet, quitting smoking, and moderating alcohol intake, can help manage the condition and lower the risk of stroke.
Chronic conditions such as hypertension, diabetes mellitus, chronic kidney disease, and thyroid disorders increase the risk of developing AFib and strokes. Proper management of these conditions is crucial in reducing the risk of AFib and associated complications.
A recent review highlights the need for a multidisciplinary, individualized approach to managing atrial fibrillation, recognizing that each patient's underlying risk factors and treatment needs may differ. By identifying and addressing the specific risk factors for each patient, healthcare providers can help manage and control atrial fibrillation long-term.
Dr. Stephen Tang, a board-certified cardiac electrophysiologist, emphasizes that managing atrial fibrillation goes beyond oral anticoagulation for stroke prevention or rate or rhythm control with medication or ablation. He states that controlling various risk factors and comorbidities is essential in achieving sustained management and control of atrial fibrillation.
Incorporating lifestyle modifications, medications, and invasive procedures, such as catheter ablation, can help restore a normal heart rhythm and reduce the risk of stroke for individuals with atrial fibrillation. Adhering to a comprehensive management plan and monitoring progress is key to achieving optimal outcomes for patients with atrial fibrillation.
- The predictive AQ score can help identify the risk of developing afib and strokes in a population.
- Depression, a common mental-health issue, is linked to an increased risk of afib and subsequent strokes.
- Science has continuously focused on understanding the complex relationship between chronic diseases like afib, hypertension, and cardiovascular health.
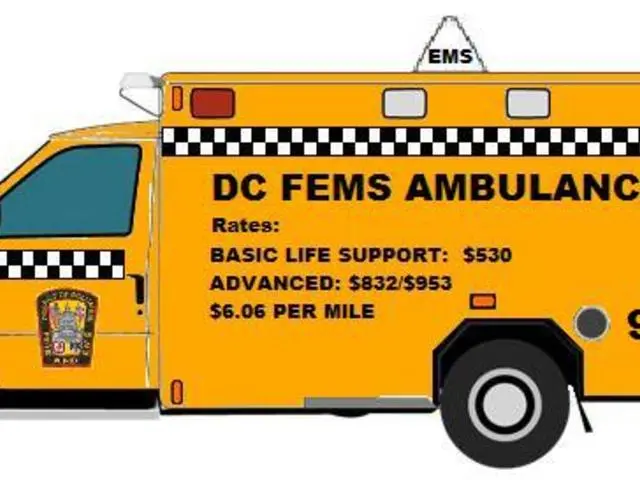
- Financial constraints can impact an individual's ability to access necessary healthcare services for managing afib and its associated risks, such as personal-finance issues like medication costs.
- Achieving and maintaining fitness-and-exercise, nutrition, and mental-health along with managing hypertension and other comorbidities are key to reducing the risk of afib and its complications.
- Nonmodifiable factors such as genetics, age, and sex can predispose someone to afib, but lifestyle choices and comorbid conditions significantly influence its prevalence and severity.
- Early detection, appropriate treatment, and ongoing management are crucial for reducing the risk of afib-related strokes and improving health-and-wellness outcomes in affected populations.
- Regular check-ups with healthcare providers can help monitor afib, manage comorbid conditions, and make necessary adjustments to the treatment plan according to the patient's specific risk factors.
- Economic factors such as insurance coverage and access to quality medical care can affect afib management and long-term outcomes among different population groups.
- A collaborative effort between patients, healthcare providers, and medical-conditions specialists is necessary to develop personalized strategies aimed at managing afib and preventing strokes.