Personalized Care for Atrial Fibrillation: Focusing on Lifestyle Modifications to Reduce Risk
Revised Article:
Atrial fibrillation (AFib) - the most common type of arrhythmia - is a complex heart condition involving an irregular heart rhythm that's a significant risk factor for stroke. Alongside well-known cardiovascular health risk factors like physical activity, diabetes, and smoking, the presence of chronic health conditions plays a crucial role. A comprehensive review gathered evidence on lifestyle factors, comorbid conditions, and socioeconomic factors that may influence the risk of AFib.
Dr. Stephen Tang, a board-certified cardiac electrophysiologist, explained, "The comprehensive management of AFib goes beyond oral anticoagulation for stroke prevention or rate or rhythm control with medication or ablation. This versatile disease is driven by numerous risk factors and comorbidities."
Genetic factors, sex, and age are nonmodifiable AFib risk factors. Modifiable factors include lifestyle choices, comorbid conditions, and socioeconomic factors.
Lifestyle changes and medications can help manage this heart condition. Blood thinners, also known as anticoagulants, can reduce the risk of blood clot formation and stroke. While drugs targeting vitamin K, such as warfarin, have been conventionally used, nonvitamin K antagonist oral anticoagulants (NOACs) have become the first-line treatment for AFib.
Physical inactivity, obesity, smoking, and high alcohol consumption intensify the risk of AFib incidence and symptom severity. Regular exercise and high-intensity interval training can reduce morbidity and improve quality of life for those with AFib. Analyses suggest that weight loss can lower the risk of AFib recurrence and complications. Obstructive sleep apnea can increase the risk of AFib and its complications, while managing sleep apnea using a continuous positive airway pressure (CPAP) machine can lower the risk.
Individuals with pre-existing cardiovascular conditions, such as coronary artery disease, hypertension, heart failure, and cardiomyopathies, are at higher risk of AFib. Poor management of hypertension significantly raised the risk of developing AFib. Diabetes positively correlates with AFib incidence and complications, though the evidence is mixed regarding control of blood glucose levels. While high total cholesterol and low-density lipoprotein levels are risk factors for cardiovascular diseases, they associate with a lower risk of AFib. In contrast, higher levels of triglycerides are associated with an increased risk of AFib.
Nearly half of all individuals with AFib show impaired kidney function, impacting anticoagulant drug metabolism and increasing the risk of adverse effects. Those with AFib and kidney disease experience more complications during catheter ablation. Short-term exposure to air pollution and chronic respiratory conditions, like COPD, are linked to an increased risk of AFib.
Mental health conditions, such as stress, depression, schizophrenia, and bipolar disorder, are associated with an increased risk of AFib. Depressive symptoms improve as the risk decreases in individuals using antidepressants. Studies suggest a lack of social support and access to healthcare may hinder optimal anticoagulant therapy utilization for AFib, which is essential for maintaining a regular heart rhythm.
In addition to these risk factors, sex, socioeconomic status, and ethnicity/race may influence the risk of AFib. Men are at higher risk than women, but women experience more severe complications, such as stroke and mortality, attributed to differences in biological factors, access to healthcare, and psychological factors like stress.
Due to the significant impact of multiple factors, individualized care tailored to each patient's specific needs is crucial to effectively manage AFib. Dr. Nikhil Warrier, a board-certified cardiac electrophysiologist, emphasized, "The underlying risk factors that increase the likelihood of poor AFib-related outcomes can be different between every patient." While many risk factors are commonly associated with cardiovascular disease, their implementation in managing AFib can present challenges due to the difficulty in altering lifestyle and habits required for prevention.
- The risk of stroke, a significant complication of Atrial Fibrillation (AFib), can be reduced through the use of blood thinners, also known as anticoagulants.
- Regular exercise and high-intensity interval training can help reduce the morbidity and improve the quality of life for individuals with AFib, while weight loss can lower the risk of AFib recurrence and complications.
- Individuals with pre-existing cardiovascular conditions, such as coronary artery disease, hypertension, heart failure, and cardiomyopathies, are at a higher risk of AFib.
- Mental health conditions, such as stress, depression, schizophrenia, and bipolar disorder, are associated with an increased risk of AFib. Depressive symptoms improve as the risk decreases in individuals using antidepressants, but a lack of social support and access to healthcare may hinder optimal anticoagulant therapy utilization for AFib.
- The presence of chronic health conditions, like diabetes, and lifestyle choices, such as physical inactivity, obesity, smoking, and high alcohol consumption, can intensify the risk of AFib incidence and symptom severity.
- Science continues to explore the links between various factors and AFib, with genetic factors, sex, and age being nonmodifiable risk factors, while lifestyle choices, comorbid conditions, and socioeconomic factors are modifiable.
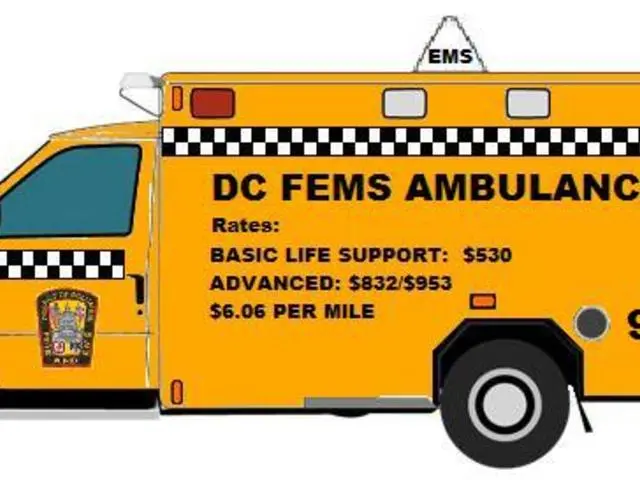
- The comprehensive management of AFib extends beyond medication and ablation, with personal-finance factors also playing a role in accessing treatment, especially for individuals in lower socioeconomic brackets.
- Consistent with the importance of health and wellness, managing nutrition, fitness, and mental health can help mitigate the risk of AFib and improve cardiovascular health, with regular check-ups and preventative measures being crucial for those at risk of this chronic disease.